ACIP Undone: Proof, Policy, and Panic Over a Hepatitis B Vaccine
- Heather McSharry, PhD

- Dec 17, 2025
- 19 min read
Summary

In this episode, we explore the science, history, and policy behind one of the most quietly successful vaccines in public health: the hepatitis B vaccine. While the virus rarely makes headlines, it causes over a million deaths each year from liver failure and cancer. We break down how the virus works, why infants are uniquely vulnerable, and how a birth-dose vaccination strategy saves lives decades before disease would ever appear. We also look at how the new antivax ACIP is destroying public trust...not because the science changed, but because ideology is overriding it.
All citations at the end of the post.
Listen here or scroll down to read full episode.
Full Episode
For decades, the U.S. had something rare and remarkable in public health: stability.
Not perfection — but a system built on evidence, expert consensus, and a shared commitment to protecting people. The FDA, CDC, and ACIP were far from anonymous acronyms — they were institutions that earned trust by acting transparently, adjusting to new science, and safeguarding health without political interference.
You didn’t have to know every study. You could rely on the fact that someone had read them, reviewed them, debated them — and made a decision based on what would protect the most people with the least harm.
But now, that foundation is being deliberately undone.
Experts are being replaced with ideologues. Evidence is being overridden by agenda. And decisions that once reflected decades of careful science are being rewritten by people who reject the entire premise of vaccination.
And when that happens — when systems that protect us are hollowed out from within — fear isn’t accidental.
It’s the predictable result.
In early December, that’s exactly what happened with one of the quietest, most successful vaccines we’ve ever made. A vaccine that prevents liver failure. A vaccine that prevents cancer. A safe vaccine that most of us received without a second thought.
Hepatitis B.
And now—not because of new data or new risk, but because long-standing safeguards around vaccine policy were deliberately dismantled—people are hearing they shouldn't trust this vaccine or need the protection it offers.
This is ACIP Undone: Proof, Policy, and Panic Over a Hepatitis B Vaccine.
So let's talk about what Hepatitis B actually is, why this vaccine matters so much, why it’s given at birth, and how this ACIP betrayal dragged this vaccine into the spotlight.
Hepatitis B is not a flashy virus. It doesn’t spread explosively through the air. It doesn’t cause dramatic hemorrhagic fevers. It doesn’t generate daily headlines.
But it is one of the most efficient, persistent, and deadly viruses we’ve ever encountered.
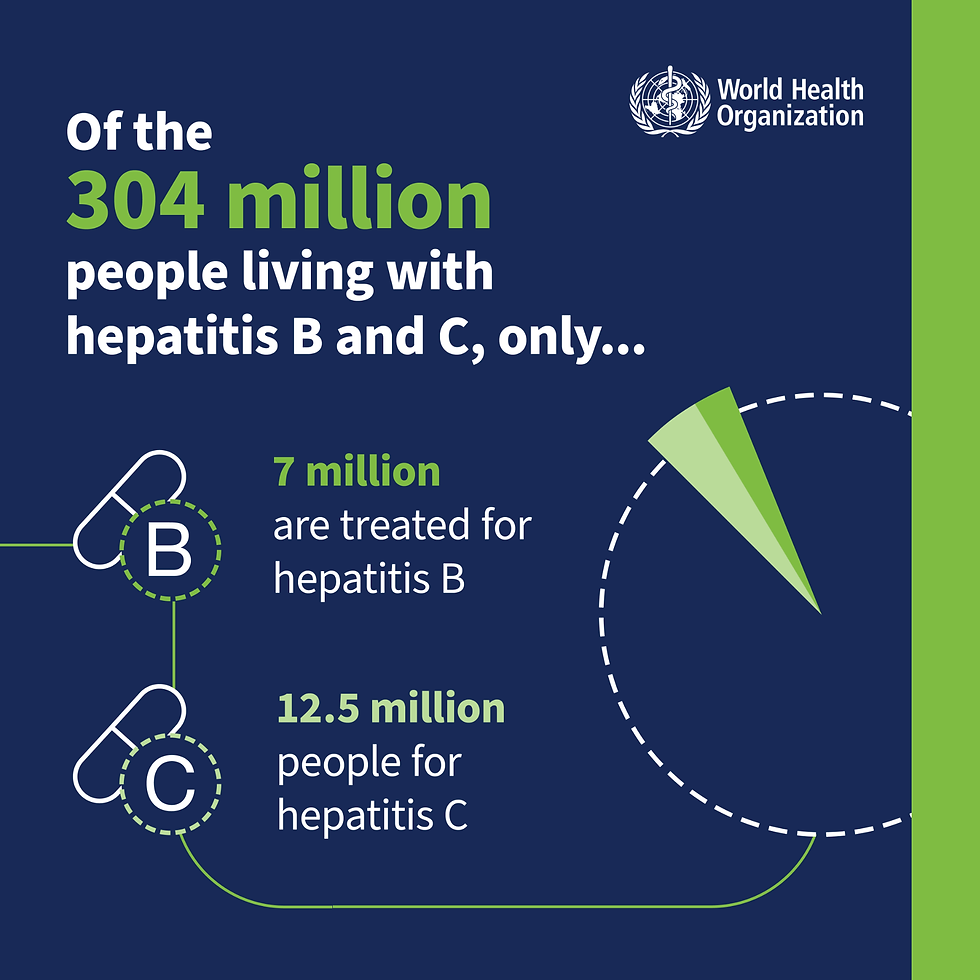
Globally, more than 250 million people are living with chronic Hepatitis B infection today. Every year, over a million people die from its long-term consequences—mostly from liver failure and liver cancer. That burden falls heaviest in parts of Asia, sub-Saharan Africa, and the Pacific Islands, but no country is untouched. In the United States alone, hundreds of thousands of people live with chronic infection, many of them undiagnosed. For data on the country you live in, check out the WHO database. Click on the country menu to select your country and it will provide the hepatitis stats available.
Hepatitis B Virology and Pathogenesis
Part of what makes Hepatitis B so dangerous is the virus itself.
Hepatitis B virus (HBV) is a small, enveloped DNA virus that belongs to the Hepadnaviridae family, genus Orthohepadnavirus. It has a partially double-stranded, circular DNA genome so compact it borders on elegant. It uses four overlapping reading frames to encode everything it needs—essentially writing multiple biological instructions on the same stretch of genetic text and it replicates through an unusual process involving reverse transcription of an RNA intermediate—making it one of the only DNA viruses to do so. This replication strategy is part of what makes HBV both persistent and difficult to eradicate once chronic infection is established.
Its target is the hepatocyte, the primary functional cell of the liver. Entry is highly specific. HBV binds to a receptor called NTCP, a bile acid transporter that normally plays a role in liver metabolism. The virus has evolved to hijack that system, giving it highly specific tropism for liver cells, meaning it has a strong preference for infecting those cells.
Once inside the cell, HBV reveals one of its unusual features: its genome is not fully double-stranded. Instead, it’s a partially double-stranded circular DNA molecule—incomplete by design.
To begin replication, the virus relies on the host cell to repair and complete the genome, converting it into a fully double-stranded form known as covalently closed circular DNA, or cccDNA. This cccDNA doesn’t integrate into the host genome. Instead, it remains in the nucleus like a durable molecular blueprint, serving as a long-lived template for viral RNA transcription.
And that persistence is the problem.
From cccDNA, the virus produces multiple RNAs and proteins. One of those RNAs—the pregenomic RNA—is packaged together with the viral polymerase inside a newly forming nucleocapsid. Inside that capsid, HBV uses reverse transcription to convert RNA back into DNA, a replication strategy that’s rare among DNA viruses.
Some of these nucleocapsids go on to form complete infectious particles. Others recycle back to the nucleus, replenishing the cccDNA pool.
This is why Hepatitis B is so hard to cure. Even when antiviral drugs suppress viral replication in the blood, the cccDNA reservoir can remain behind, ready to restart infection.
HBV also floods the system with decoys.
In addition to complete viral particles, infected cells release massive quantities of empty surface-antigen particles—essentially shells without genetic material. These circulate in the bloodstream and soak up immune attention, helping the virus evade clearance while real infection continues quietly in the background.
One viral protein shows up again and again in discussions of HBV pathogenesis: HBx.
HBx is a regulatory protein required for efficient viral replication in human hepatocytes. It doesn’t directly cause cancer, but it interferes with host signaling pathways involved in cell cycle control, metabolism, DNA repair, and apoptosis.
Fragments of HBV DNA can also integrate into the host genome—particularly in the setting of chronic infection. This integration doesn't involve the stable cccDNA form, which remains episomal, that means it quietly stays in the nucleus and fuels chronic infection. What Integration does involve are incomplete DNA intermediates from the viral replication process. While these fragments do not support full viral replication, they can continue to express viral proteins, including HBx, which may disrupt normal cellular functions and contribute to the development of hepatocellular carcinoma.
Transmission of Hepatitis B reflects this biology.
HBV is present in blood and certain body fluids. It spreads during childbirth from an infected parent to a newborn. It spreads through sexual contact. It spreads through shared needles, needlestick injuries, and medical procedures when infection control fails.
It can also persist at very low levels. Some people have what’s called occult Hepatitis B infection—where viral DNA is detectable, but standard surface antigen tests are negative—complicating diagnosis and surveillance.
And unlike viruses that cause immediate, obvious illness, Hepatitis B often enters quietly.
Many adults experience mild or even asymptomatic acute infections. About 90 to 95 percent of adults will clear the virus. But infants and young children are different.
If a baby is infected at birth, the immune system often doesn’t clear the virus. No fever. No dramatic illness. Just a virus that stays.
Chronic Hepatitis B doesn’t kill quickly. It injures the liver slowly, over decades, through repeated cycles of immune-mediated inflammation. Fibrosis progresses to cirrhosis. Liver function declines. And the constant pressure of cell damage and regeneration dramatically increases the risk of hepatocellular carcinoma—one of the deadliest cancers worldwide.
Which brings us to one of the greatest successes in public health history.
The Hepatitis B vaccine.
But before we go into the vaccine let's clear up some things about Hep B and the other
hepatitis viruses. There are three:
Hepatitis A causes a short-term digestive illness spread through food and water — it clears on its own, and we have a vaccine.
Hepatitis B is a bloodborne virus that often goes unnoticed but can lead to lifelong infection, liver failure, and cancer — and the vaccine given at birth can prevent all of that.
Hepatitis C spreads mostly through blood, especially from needles. It can lead to chronic liver disease and cancer, but we don’t have a vaccine yet — though treatment is curative.
So why the fuss over Hep B if Hep C causes the same problems and has no vaccine and that's fine?
It’s true — both Hepatitis B and Hepatitis C can cause chronic infection, liver failure, and cancer. But here’s the difference: Hepatitis B can be prevented before exposure — with a safe, effective vaccine given at birth. Hepatitis C can’t. And when you look closely, Hepatitis B is not just equivalent to Hep C — in many ways, it’s worse. Hepatitis B is far more infectious — about 100 times more contagious than HIV, and more transmissible than Hep C through birth, blood, and even household contact. It’s also far more likely to become chronic in infants: If a baby is infected with Hepatitis B at birth, they have a 90% chance of developing lifelong infection. With Hepatitis C, that number is around 5–15%. And even though we don’t have a vaccine for Hep C, we do have a cure — highly effective antiviral pills that can eliminate the virus in just a few weeks. Hepatitis B can’t be cured. Its viral DNA creates a permanent blueprint in the liver’s cells. Treatment can suppress it, but not erase it. So yes — both viruses are dangerous. But Hepatitis B is harder to cure, easier to spread, more damaging in infants, and completely preventable with a vaccine that works. That’s not “a fuss.” That’s what public health is supposed to do: stop harm before it happens.
Back to the Hep B vaccine.
There are currently two hepatitis B vaccines approved for use at birth in the United States—Engerix-B® and Recombivax HB®. Both are recombinant vaccines that contain only the surface antigen of the virus, and both are highly effective and well-studied in newborns.
These are the vaccines used for the first dose given in the hospital shortly after birth. Ideally within the first 24 hours of life, which is critical for preventing perinatal transmission. For later doses in the series, infants may receive the same vaccine—or a combination vaccine like Pediarix®, which includes protection against hepatitis B along with DTaP and polio.
And for adults, there’s a newer option called Heplisav-B®, which uses a novel adjuvant and is given as a two-dose series—and it’s not approved for use in infants.
This vaccine doesn’t just reduce risk.
It prevents chronic infection. It interrupts the progression to liver disease. It protects against liver failure. And it dramatically lowers the risk of liver cancer.
It doesn’t just change one outcome — it changes the trajectory of a person’s life.
It is, quite literally, a cancer-preventing vaccine.
And we’ve known that for decades.
For more than thirty years, routine screening for Hepatitis B during pregnancy and universal vaccination of infants at birth have been the cornerstone of Hepatitis B prevention in the United States. This strategy didn’t emerge casually. It came out of repeated, systematic reviews of safety, effectiveness, and real-world impact.
And every time ACIP reviewed the evidence, the conclusion was the same.
The birth dose matters.
In fact, the universal birth dose recommendation was first issued in 1991 by the CDC and the American Academy of Pediatrics, after years of rising concern that the high-risk, targeted approach was failing to protect infants.
That shift to universal vaccination at birth—regardless of maternal risk factors—became a defining success in U.S. public health. Since then, hepatitis B infections among children and adolescents have dropped by over 99%, and rates of chronic infection have plummeted. This isn’t a new idea. It’s a proven one.
Hepatitis B is not a lifestyle virus. It’s not a morality virus. It’s a virus that exploits blood exposure, immune immaturity, and gaps in systems of care.
And newborns are uniquely vulnerable.
The birth dose exists for one reason—timing.
Not every pregnant person is tested. Some tests miss recent infections. Some results aren’t communicated. Some births happen outside ideal medical settings. And even when everything goes right, follow-up can fail.
The virus doesn’t wait for paperwork.
The birth dose creates a firewall. It protects the infant before exposure can occur. It closes the gap between risk and detection.
And we know this works.
But in recent weeks, lies about the hepatitis B vaccine are gaining traction online—including that it was only tested on 147 newborns for five days, with no placebo group.
That is false. And here’s the truth:
The hepatitis B vaccine underwent rigorous, large-scale clinical trials long before it became routine. One Phase III trial in Vietnam compared two vaccine formulations in healthy newborns and found them both safe and effective—monitoring wasn’t five days, but months. That study was just one of many.
Long-term studies have tracked vaccinated children for over a decade, confirming durable protection and no unexpected safety concerns. Trials in infants born to hepatitis B-positive mothers—those most at risk—showed that combining the hepatitis B vaccine with hepatitis B immune globulin (HBIG) reduced infection rates by more than 90 percent. HBIG is a concentrated solution of protective antibodies, derived from donated human plasma, that provides immediate, short-term passive immunity. It acts as a biological shield, protecting the newborn while their immune system begins developing its own long-term defense in response to the vaccine.
Multiple independent studies across continents, from the U.S. to China to Vietnam, involved thousands of infants. No single five-day trial, no mystery data, and certainly no evidence of hidden harm.
These lies thrive on omission. They cherry-pick an early-phase trial and ignore the 40 years of data that followed. Like all medical interventions, the vaccine isn’t completely risk-free—but the risks are minimal, well-characterized, and far outweighed by its benefits. After hundreds of millions of doses and decades of safety surveillance, no serious safety signals have been causally linked. The science is clear, and the evidence is public. This vaccine is one of the most studied and safest we have ever developed.
And independent reviews of decades of data show that the hepatitis B vaccine birth dose is safe. Evidence from randomized trials, national surveillance systems, and long-term follow-up studies consistently shows only expected, mild reactions—things like brief fever or redness of the injection site. No short-term or long-term serious adverse events, and no causally linked deaths have been identified in large-scale post-marketing surveillance.
When researchers directly compared infants vaccinated at birth with those vaccinated later, there was no difference in adverse event rates.
Delaying the first dose did not make vaccination safer. What it did was reduce protection.
The birth dose is highly effective. Vaccination alone reduces perinatal transmission by about 70 percent in infants born to infected mothers. When the birth dose is combined with HBIG, protection exceeds 90 percent—as shown earlier. About one-quarter of infants develop protective antibody levels after the first dose, and roughly 95 percent are protected after completing the full series.
Long-term studies show immune protection lasting at least 35 years. And there is no evidence that delaying the first dose improves immune response.
Just the opposite.
Universal birth-dose vaccination has been foundational to the dramatic decline in Hepatitis B infections in U.S. children—and the reductions we now see in adults reflect protection that began in infancy.
Now, some critics of the hepatitis B birth dose try to flip the logic and say:
“If late pregnancy infection is such a big concern, why don’t they also give hepatitis B immune globulin—HBIG—to all newborns? Clearly, it must not be that serious.”
But that completely misunderstands both the science and the public health strategy.
HBIG is not a scalable tool for universal prevention. It's is a passive immune product made from donated human plasma. It provides short-term protection, not long-term immunity. It’s used strategically—in newborns at highest risk, like those born to mothers known to be hepatitis B-positive—because it gives those infants an immediate antibody shield while the vaccine begins to build lasting protection.
But here’s why we don’t give HBIG to everyone:
It’s not needed for most infants. The hepatitis B vaccine alone is highly effective at preventing infection in newborns without additional intervention. That’s why it’s used as the foundation of protection for all infants.
HBIG is reserved for high-risk situations. It’s specifically used in babies born to mothers known to be hepatitis B-positive—those most likely to have been exposed at birth—because it provides immediate protection while the vaccine takes effect.
It’s a resource-intensive product. HBIG is derived from donated human plasma, which requires rigorous screening, complex processing, and cold storage. Widespread use for all newborns would strain limited supplies and potentially divert it from infants who truly need it most.
So no—the fact that HBIG isn’t given to every newborn doesn’t mean late pregnancy infection isn’t a concern. It means public health experts are using the right tool for each level of risk.
The birth dose provides long-term, population-wide protection.
HBIG provides immediate, targeted backup.
And trying to use the HBIG policy to discredit the birth dose is like arguing we shouldn’t wear seatbelts because not everyone needs an airbag. It’s a fundamental misunderstanding of how prevention works.
Together, they work. The science backs it. The outcomes prove it. And the only thing the critics are revealing is that they haven’t read the evidence.
What's In the Hep B Vaccines?
Now—let’s open the vial.
All hepatitis B birth dose-approved vaccines are recombinant subunit vaccines, in fact all Hep B vaccines are recombinant subunit vaccines. They vary by dose, not antigen type. Recombinant subunit vaccines don’t contain live virus or killed virus. And they cannot cause hepatitis B infection.
Instead, they contain a single viral component: hepatitis B surface antigen, or HBsAg. This is the outer protein that normally coats the virus—the part the immune system needs to recognize to stop the virus.
That antigen is made using recombinant DNA technology in yeast cells, which act as biological factories to produce large quantities of one specific protein. There is no viral genome involved. No replication. No persistence.
Because a protein alone doesn’t always produce a strong immune response, the vaccine includes an adjuvant. In hepatitis B vaccines, that adjuvant is an aluminum salt—usually aluminum hydroxide or aluminum phosphate. Its job is to help the immune system pay attention, allowing a small amount of antigen to generate durable immunity.
The amount of aluminum in a hepatitis B vaccine dose is small—well within established safety limits—and less than what infants naturally ingest from breast milk or formula in the first days of life.
The vaccine also contains stabilizers—salts and buffering agents—to keep the antigen intact during manufacturing, storage, and transport.
Single-dose hepatitis B vaccines used for routine infant immunization do not contain preservatives.
There are trace residuals from the manufacturing process—tiny amounts of yeast proteins or other substances used during purification. These are present at levels so low they have no biological effect.
That’s the vial.
That’s everything in it, and why it’s there.
And here's a summary of the vaccine components for your convenience:
Hepatitis B Vaccines—Inside the Vial
Type of Vaccine: Recombinant subunit vaccine—uses a purified viral protein as antigen
Ingredients:
Antigen—the pathogen or part of the pathogen that elicits the immune response
All hepatitis B vaccines used in the United States contain hepatitis B surface antigen (HBsAg). This is a single viral protein that forms the outer surface of the hepatitis B virus.
HBsAg is produced using recombinant DNA technology, typically in yeast cells (Saccharomyces cerevisiae), which act as biological factories to manufacture the protein. The antigen cannot cause hepatitis B infection because it contains no viral genome and cannot replicate.
Common U.S. products (infant/adult formulations vary by dose, not antigen type):
Engerix-B®
Recombivax HB®
Heplisav-B® (adult-only, different adjuvant)
Pediarix® (combination vaccine containing Hep B + DTaP + IPV)
Adjuvant—a substance that enhances the body’s immune response to the antigen
Most hepatitis B vaccines contain an aluminum salt adjuvant, typically aluminum hydroxide or aluminum phosphate.
The adjuvant helps stimulate a stronger and longer-lasting immune response, allowing a small amount of antigen to generate effective immunity.
Aluminum salts have been used in vaccines for decades.
The amount of aluminum in a hepatitis B vaccine dose is small and within established safety limits.
Infants are exposed to more aluminum from breast milk, formula, and food in the first days of life than from the vaccine.
Note: Heplisav-B® uses a different adjuvant (CpG 1018, a synthetic DNA sequence that stimulates innate immunity) and is approved only for adults, not infants.
Stabilizers—to help the vaccine maintain effectiveness during manufacturing, storage, and transport
Hepatitis B vaccines contain stabilizing agents that help maintain the integrity of the antigen.
Depending on the product, these may include:
Salts (such as sodium chloride)
Buffers to maintain pH
These substances have no pharmacologic activity and are present only to keep the vaccine stable and effective.
Preservative—to protect the vaccine from contamination
Single-dose hepatitis B vaccine vials do not contain preservatives.
Multi-dose vials used in the past contained thimerosal, but routine infant hepatitis B vaccines in the U.S. are now preservative-free.
Delivery Components:
None.
The vaccine is administered as a sterile intramuscular injection and does not contain delivery devices, nanoparticles, or viral vectors.
Residuals:
Remember: residuals are trace byproducts from the manufacturing process with no medicinal function. They are removed during purification, and any remaining amounts are extremely small.
Depending on the vaccine product, residuals may include:
Trace yeast proteins from the recombinant production process
Trace formaldehyde used during manufacturing (well below naturally occurring levels in the human body)
Trace proteins or buffers used during purification
These residuals are present at levels far below those known to cause harm.
Diluent / Suspension Medium:
Hepatitis B vaccines are supplied as a liquid suspension and do not require reconstitution. The vaccine is suspended in sterile water or saline solution for injection.
For more details on these components, please check out the Inside the Vial episode. It goes more in-depth on what each component does and how we know they are safe. Links to product inserts and all relevant studies are at the end of the post.
OK, so for infants, hepatitis B vaccination is given as a three-dose series. The first dose is given at birth. The second dose follows at one to two months of age, and the third at six months. And just so we're clear, this schedule has been recommended for decades by ACIP until experts on ACIP were replaced with antivax ideologues.
After the full series, about 95 percent of healthy infants and children develop protective antibody levels. Protection lasts for decades. Even when measurable antibodies decline, immune memory remains. For most people, the full infant series provides lifelong protection. Routine boosters aren’t needed unless a person is immunocompromised or has specific clinical risks.
This vaccine doesn’t rush the immune system. It trains it.
And this is why hepatitis B vaccination has changed the trajectory of disease—by preventing chronic infection, liver failure, and cancers that would have appeared years or decades later.
Now—with the science and the contents on the table—let’s talk about what was done.
ACIP's Betrayal
When ACIP’s expert-driven process was replaced with ideologically-aligned leadership, the science didn’t change.
What changed was that overwhelming evidence and expert input—from clinicians, public health leaders, and hepatitis B specialists—was ignored.
The hepatitis B vaccine did not suddenly become unsafe. No efficacy signal disappeared. No new harm emerged.
But who controls the process matters.
Public trust depends on decisions being made by qualified experts, using evidence transparently, without political interference. When that is replaced by ideology-driven disinformation, vaccine policy stops being about health and starts being about power.
And disinformation isn’t accidental. It’s weaponized misinformation. It’s strategic. And once trust is deliberately eroded, facts have a harder time reaching the people who need them most.
That’s the real damage of abandoning evidence-based governance in public health. It doesn’t erase decades of evidence—but it blocks that evidence from reaching the people whose lives depend on it.
Hepatitis B vaccination is one of the clearest examples of prevention done right. It protects infants before harm occurs. It saves lives quietly. It prevents cancers people never know they avoided. And it deserves better than to be deliberately undermined by people entrusted with protecting public health.
And when evidence-based systems are intentionally weakened, it’s on all of us—scientists, clinicians, and communicators—to name that clearly and steady the ground for the people caught in the fallout.
This wasn’t a vaccine failure.
It was a betrayal.
Talk to your doctor about vaccinating your newborn. And if your doctor discourages the hepatitis B vaccine, ask to see the evidence behind their recommendation.
If you're unsure whether what you're being told is credible, reach out. I have an entire episode on how to spot misinformation, and I’d be happy to help you make sense of it.
Support physicians who practice evidence-based medicine—who understand that science grows through careful study, consensus, and revision. Yes, opinions can change as we learn more. That’s not a weakness. That’s the strength of science.
But a doctor who refuses to consider overwhelming evidence—who ignores decades of research, global data, and expert consensus—is not protecting your child. They're putting them at risk. And in doing so, they come dangerously close to violating the oath to do no harm.
The take home message here is that nothing about the virus changed. Nothing about the vaccine changed. What changed is who is telling the story. And keep in mind, the people on ACIP who voted to remove these protections from newborns, were themselves safely vaccinated and protected against HBV as infants by decades of evidence-based policy. The newborns they are condemning didn't get a vote.
The good news? Some states are stepping up. In September 2025, California, Oregon, and Washington launched the West Coast Health Alliance to counter federal interference and uphold evidence-based vaccine guidance for their residents. Around the same time, seven Northeastern states and New York City formed the Northeast Public Health Collaborative, with Vermont and Washington, DC also announcing protections.
These coalitions are designed to ensure residents still have access to vaccines—and to provide recommendations based on science, not politics.
If your state hasn’t acted yet, now is the time to speak up. Tell your governor: Protect access. Trust the data. Reject disinformation. Because we can’t afford to let ideology undo decades of progress.
Thanks for being part of this discussion. If it was helpful, send it to a friend who might also find the information helpful.
Next week is Christmas and we have a special Outbreak After Dark Episode for you for that and for New Years we're talking with a biorisk expert about what bioweapons are and what they're not. Until then, stay healthy, stay informed, and spread knowledge not diseases.

References: Hepatitis A, B, and C – Effectiveness, Safety, Policy, and Biology
When key peer-reviewed articles are behind publisher paywalls, Infectious Dose provides publicly accessible PDFs for transparency and educational use.
Hepatitis B
Abers M S, Ulrich A K, and Walensky R P. 2025. Universal hepatitis B vaccination at birth—Risks of revising the recommendation. JAMA. https://jamanetwork.com/journals/jama/article-abstract/2842435 [PDF Download]
Iannacone M, Guidotti LG. 2022. Immunobiology and pathogenesis of hepatitis B virus infection. Nat Rev Immunol. https://www.nature.com/articles/s41577-021-00549-4 [PDF Download]
Beasley R P, et al. 1981. Hepatocellular carcinoma and hepatitis B virus: A prospective study of 22,707 men in Taiwan. The Lancet. https://doi.org/10.1016/S0140-6736(81)90585-7 [PDF Download]
Chang M H, et al. 1997. Universal hepatitis B vaccination in Taiwan and the incidence of hepatocellular carcinoma in children. New England Journal of Medicine. https://doi.org/10.1056/NEJM199706263362602
Schillie S, et al. 2018. Prevention of hepatitis B virus infection in the United States: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recommendations and Reports. https://www.cdc.gov/mmwr/volumes/67/rr/rr6701a1.htm
Hyams K C. 1995. Risks of chronicity following acute hepatitis B virus infection: A review. Clinical Infectious Diseases. https://doi.org/10.1093/clinids/20.4.992 [PDF Download]
Qiu, J., et al. 2024. Efficacy and safety of hepatitis B vaccine: an umbrella review of meta-analyses. Expert Review of Vaccines. https://www.tandfonline.com/doi/full/10.1080/14760584.2023.2289566#abstract
Gidengil C, et al. 2021. Safety of vaccines used for routine immunization in the United States: An updated systematic review and meta-analysis. Vaccine. https://www.sciencedirect.com/science/article/abs/pii/S0264410X21003856 [PDF Download]
Schwarz T.F., et al. 2019. Long-term antibody persistence against hepatitis B. Human Vaccines & Immunotherapeutics. https://pmc.ncbi.nlm.nih.gov/articles/PMC6363144/
Hieu, N.T., Sarnecki, M., and Tolboom, J. 2015. The Safety and Immunogenicity of Two Hepatitis B Vaccine Formulations (Thiomersal-free and Thiomersal-containing) in Healthy Vietnamese Infants: A Phase III, Prospective, Single-blinded, Randomized, Controlled Trial. The Pediatric Infectious Disease Journal https://journals.lww.com/pidj/fulltext/2015/01000/the_safety_and_immunogenicity_of_two_hepatitis_b.17.aspx
Chen, Z, et al. 2020. Antenatal administration of hepatitis B immunoglobulin and hepatitis B vaccine to prevent mother to child transmission in hepatitis B virus surface antigen positive pregnant women: A systematic review and meta-analysis. Medicine. https://journals.lww.com/md-journal/fulltext/2020/04170/antenatal_administration_of_hepatitis_b.99.aspx
Post-Marketing Safety and Policy Implementation
Zhou W, et al. 2004. Surveillance for safety after immunization: Vaccine Adverse Event Reporting System (VAERS)—United States, 1991–2001. MMWR Surveillance Summaries. https://www.cdc.gov/mmwr/preview/mmwrhtml/ss5201a1.htm
Weng M K, et al. 2022. Universal hepatitis B vaccination in adults aged 19–59 years: Updated recommendations of the ACIP. MMWR. https://www.cdc.gov/mmwr/volumes/71/wr/mm7113a1.htm
World Health Organization. 2017. Hepatitis B vaccines: WHO position paper – July 2017. Weekly Epidemiological Record. https://www.who.int/publications/i/item/who-wer9227
World Health Organization. Global Hepatitis Report 2024. https://www.who.int/publications/i/item/9789240054279 Scroll down for report or dowload here: [PDF Download]
U.S. Food and Drug Administration.
Recombivax HB Product Page. https://www.fda.gov/media/87994/downloadU.S.
Engerix-B Product Page.
https://www.fda.gov/vaccines-blood-biologics/vaccines/engerix-b
Hepatitis A
World Health Organization Immunization, Vaccines and Biologicals (IVB). 2009. The global prevalence of hepatitis A virus infection and susceptibility: A systematic review. https://www.who.int/publications/i/item/the-global-prevalence-of-hepatitis-a-virus-infection-and-susceptibility
Hepatitis C
Thomas DL. 2019. Global Elimination of Chronic Hepatitis.
New England Journal of Medicine. https://www.nejm.org/doi/full/10.1056/NEJMra1810477 [PDF Download]
.png)




Comments